Introduction: A Silent Threat and a Potential Shield
Imagine a key that could unlock a stronger, more resilient brain—a key that might be hiding in your kitchen pantry. For years, we’ve heard that Omega-3 fatty acids are “good for you,” but emerging research suggests they might be especially crucial for women’s brain health. Alzheimer’s disease casts a long shadow, affecting millions globally, but it doesn’t affect everyone equally. Women are disproportionately burdened; they are not only more likely to develop Alzheimer’s but also often face faster cognitive decline once diagnosed. Could something as simple as a dietary adjustment help shift this balance? Recent studies indicate that Omega-3 fatty acids—particularly those found in fatty fish and certain plants—might be a powerful tool in helping to protect women from Alzheimer’s disease. This isn’t just another health fad; it’s a compelling intersection of cutting-edge science, gender-specific medicine, and everyday lifestyle choices. Let’s dive into the fascinating world of fats, brains, and why women might need to pay special attention.
Understanding Omega-3 Fatty Acids: More Than Just Fish Oil

Omega-3 fatty acids are a family of essential polyunsaturated fats that play critical roles in the human body. The term “essential” means our bodies cannot produce them efficiently, so we must obtain them through diet or supplementation. The three primary types are:
ALA (Alpha-linolenic acid): Found in plant sources like flaxseeds, chia seeds, walnuts, and canola oil. ALA serves mainly as a precursor to EPA and DHA, though the conversion rate in the human body is relatively low.
EPA (Eicosapentaenoic acid): Found primarily in marine sources, especially oily fish like salmon, mackerel, and sardines. EPA is known for its anti-inflammatory properties.
DHA (Docosahexaenoic acid): Also found in marine sources, DHA is a major structural component of the brain, retina, and many other tissues. It is crucial for brain development and function.
The brain is about 60% fat, and DHA alone makes up about 30% of the fatty acids in the gray matter. It supports neuronal structure, facilitates communication between brain cells, and possesses anti-inflammatory and antioxidant properties. These functions are vital for maintaining cognitive health and may help protect against neurodegenerative processes like those seen in Alzheimer’s disease .
The Gender Gap in Alzheimer’s Disease: Why Women Are More Vulnerable
Alzheimer’s disease is the most common form of dementia, and it doesn’t affect men and women equally. Globally, women account for nearly two-thirds of all Alzheimer’s cases. For decades, this disparity was largely attributed to women’s longer life expectancy. However, research now suggests that longevity alone doesn’t fully explain the difference. Biological, genetic, and hormonal factors likely contribute to women’s heightened vulnerability:
Hormonal Changes: The decline in estrogen during menopause may play a role. Estrogen has neuroprotective effects, and its reduction might make the brain more susceptible to damage.
Genetic Factors: The APOE4 allele is the strongest genetic risk factor for late-onset Alzheimer’s disease. Some research suggests that the APOE4 gene might have a more pronounced effect in women than in men .
Brain Structure and Metabolism: Differences in brain connectivity, glucose metabolism, and even the accumulation of amyloid plaques have been observed between men and women with Alzheimer’s.
Understanding this gender gap is crucial because it means prevention and treatment strategies might need to be sex-specific. This is where Omega-3 enters the picture.
Groundbreaking Research: The 2025 King’s College London Study
A landmark study published in 2025 brought the relationship between Omega-3 and women’s brain health into sharp focus. Researchers at King’s College London analyzed blood samples from 841 participants—306 with Alzheimer’s, 165 with mild cognitive impairment, and 370 cognitively healthy controls. The findings were striking:
Women with Alzheimer’s disease had up to 20% lower levels of unsaturated fats, including Omega-3 fatty acids, compared to cognitively healthy women.
This pattern was not observed in men with Alzheimer’s, suggesting a unique sex-specific metabolic component to the disease.
The study also found that women with Alzheimer’s had higher levels of saturated fats, further hinting at a disrupted lipid metabolism profile.
Dr. Cristina Legido-Quigley, a senior author of the study, noted, “The difference between the sexes was the most shocking and unexpected finding… There’s an indication that having less of these compounds could be causal in Alzheimer’s, but we need a clinical trial to confirm that” .
This research suggests that for women, maintaining adequate Omega-3 levels might be particularly critical for brain health. The study implies that the disease process in women might be linked to how their bodies metabolize and utilize these essential fats, potentially due to hormonal influences or genetic factors.
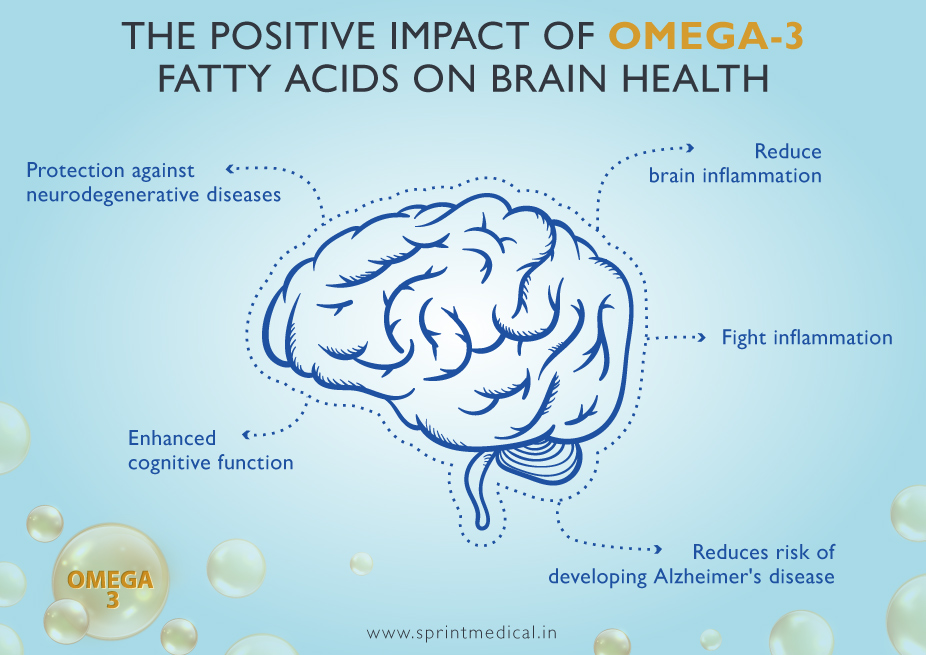
How Omega-3 Fatty Acids Protect the Brain: Mechanisms of Action
The potential benefits of Omega-3 for brain health are supported by a robust body of research detailing several protective mechanisms:
Reducing Neuroinflammation: Chronic inflammation is a key driver of Alzheimer’s disease. EPA, in particular, helps reduce the production of inflammatory molecules in the brain.
Supporting Neuronal Structure: DHA is a primary building block of neuronal membranes. Adequate DHA levels help maintain membrane fluidity, which is essential for efficient communication between brain cells.
Combating Amyloid Plaques: Some animal and cell studies suggest that DHA can help reduce the accumulation of amyloid-beta peptides, the toxic proteins that form plaques in the brains of Alzheimer’s patients .
Improving Vascular Health: Omega-3s are known to support cardiovascular health by improving blood flow, reducing triglycerides, and lowering blood pressure. Since a healthy heart and blood vessels are crucial for supplying oxygen and nutrients to the brain, this indirectly supports cognitive function.
Antioxidant Effects: DHA and EPA can help reduce oxidative stress, another contributor to neuronal damage in Alzheimer’s.
These mechanisms highlight why Omega-3 is more than just a “good fat”; it’s a multi-faceted player in maintaining cognitive resilience.
The APOE4 Gene, Omega-3, and a Personalized Approach
The APOE4 gene variant presents a fascinating complexity in the Omega-3 and Alzheimer’s story. Carrying one or two copies of APOE4 significantly increases Alzheimer’s risk. Interestingly, some studies suggest that the protective effects of Omega-3 might be strongest in APOE4 carriers, a group that already faces higher risk .
A 2024 clinical trial from Oregon Health & Science University (OHSU) provided compelling evidence for this. The study found that while fish oil supplementation didn’t show a significant benefit for all older adults, APOE4 carriers who took fish oil showed a “dramatic reduction in the breakdown of brain cell integrity” after just one year .
This points toward a future of personalized nutrition. For women, especially those with a family history of Alzheimer’s or who know they carry the APOE4 allele, ensuring adequate Omega-3 intake could be a particularly strategic part of a brain-healthy lifestyle.
Dietary Sources vs. Supplements: What’s the Best Approach?
When it comes to boosting your Omega-3 intake, you have two main options: food sources and supplements. Each has its advantages.
Dietary Sources of Omega-3
The most effective way to get EPA and DHA is through marine sources. The NHS recommends eating two 140g servings of fish per week, one of which should be oily .
Excellent Sources of EPA/DHA: Salmon, mackerel, sardines, herring, anchovies, and trout.
Good Sources of ALA: Flaxseeds, chia seeds, walnuts, hemp seeds, and edamame.
Omega-3 Supplements
For those who don’t regularly consume fish, supplements can be a practical alternative. Common options include:
Fish Oil: Contains both EPA and DHA.
Algal Oil: A vegan-friendly source derived from algae, rich in DHA.
Krill Oil: Another source of EPA and DHA, sometimes touted for better absorption.
Food First, but Supplements Can Help
The “food-first” approach is generally recommended because whole foods provide a complex matrix of nutrients that work synergistically. For example, fatty fish also provides vitamin D, selenium, and protein. However, high-quality supplements can help bridge nutritional gaps, especially for individuals with dietary restrictions or increased needs.
Beyond Omega-3: The Importance of a Holistic Diet
While Omega-3 is promising, it’s not a magic bullet. Brain health is supported by an overall healthy dietary pattern. The Mediterranean diet is often highlighted as one of the best for cognitive function. It emphasizes:
Abundant fruits, vegetables, whole grains, legumes, and nuts.
Olive oil as the primary fat source.
Moderate consumption of fish and poultry.
Limited intake of red meat, sugar, and processed foods.
This diet is naturally rich in Omega-3 (from fish and nuts), antioxidants, and anti-inflammatory compounds. A large study suggested that adhering to a Mediterranean diet could reduce dementia risk by up to 23% . This underscores that Omega-3 is most powerful as part of a broader, nutrient-dense diet.
Practical Tips: Incorporating More Omega-3 Into Your Life
Increasing your Omega-3 intake doesn’t require a complete lifestyle overhaul. Here are some simple, actionable tips:
Start with Small Fish Swaps: Replace one meat-based meal per week with a serving of oily fish. Try canned sardines on whole-grain toast for a quick lunch.
Boost Your Breakfast: Add a tablespoon of ground flaxseed or chia seeds to your yogurt, oatmeal, or smoothie.
Snack Smart: Keep a stash of walnuts for a brain-healthy snack.
Read Supplement Labels: If you choose a supplement, look for one that provides a combined EPA/DHA dose of at least 500-1000 mg. Consult with a healthcare provider, especially if you are on blood-thinning medications.
Cook with Canola or Olive Oil: While not high in Omega-3, these are healthier fat choices that support overall heart and brain health.
Conclusion: Empowering Women’s Brain Health Through Nutrition
The compelling research from King’s College London and other institutions offers a powerful message: Omega-3 fatty acids may be a critical, and often overlooked, factor in helping to protect women from Alzheimer’s disease. The striking sex differences found in these studies highlight the urgent need for more gender-specific research in neurology and nutrition.
While more research, particularly long-term clinical trials, is needed to fully confirm a causal relationship and establish definitive dosage guidelines, the current evidence is strong enough to act upon. For women, prioritizing Omega-3 intake—through a diet rich in fatty fish and plant sources or with high-quality supplements—is a proactive, science-backed strategy to support lifelong cognitive health.
Protecting your brain isn’t about a single miracle food or pill. It’s about a holistic approach that includes a nutrient-rich diet, regular physical activity, quality sleep, and social engagement. But ensuring adequate Omega-3 might just be one of the most important and empowering steps a woman can take for her brain.
What are your thoughts? Have you considered your Omega-3 intake as part of your brain health strategy? Share your experiences or questions in the comments below! For more actionable tips on leveraging nutrition for cognitive health, subscribe to our newsletter and never miss an update.